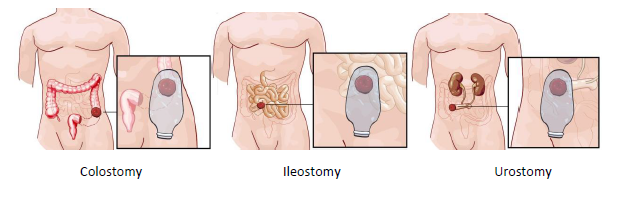
The word ‘Stoma’ comes from the Greek word that means ‘mouth’ or ‘opening’. A stoma is an artificial opening in the bowel created to bring the bowel to the surface of the abdomen, diverting the flow of faeces or urine1. There are three types of stoma, and the most common are:
- Colostomy is an opening into the colon;
- Ileostomy opens to the ileum;
- Urostomy is an opening into the urinary tract1.
The Three Types of Stoma:
People will need a stoma for many different reasons, and a stoma can be temporary or permanent depending on its need. Medical conditions such as inflammatory bowel disorders or cancer of the bowel, rectum or pelvis requiring surgical intervention may require a stoma as part of the treatment plan.
Surgery is often performed by specialist colorectal surgeons and can be done by keyhole with a faster recovery.
After surgery, a stay in hospital for between 3-10 days is usual, and a stoma nurse will advise how to manage the stoma on returning home. Life will be adjusted to live with a stoma and can be daunting at first, but it does not mean a person cannot live a full and active life.
The physical aspects of stoma formation can directly impact psychosocial function and quality of life.
To overcome the impact of stoma formation, patients may need to adopt to a process of acceptance and adjustment2. Healthcare professionals need to consider psychosocial well-being and physical health to deliver balanced, effective care that enables patients to resume a fulfilling life.
Kate* had an ileostomy formation 30 years ago due to hereditary bowel disease at the age of 29. Kate’s dad also had the same condition. He struggled to come to terms with living with his stoma, so when elective surgery was recommended, and she decided it was her best treatment choice, she chose to control her stoma.
Kate says it is essential to get the proper support from the beginning, ensuring it becomes part of daily life, like brushing your teeth each morning. She says you get to know your stoma as you learn to listen to your body.
